You have a bad posture..
Does pointing out postural discrepancies help or harm?
I, like many of you were taught to assess a patient’s posture, and was taught that if someone had an anterior pelvic tilt, then it must mean their hip flexors are short and tight and their glutes are long and weak, or if their shoulders were internally rotated, their pecs are tight and scapula retractors are long and weak. This classic “upper and lower cross syndrome”, (which is a made-up syndrome) is an overly simplistic approach that just makes a patient feel like they have something wrong with them and they need to be ‘fixed’.
If only it was that simple…
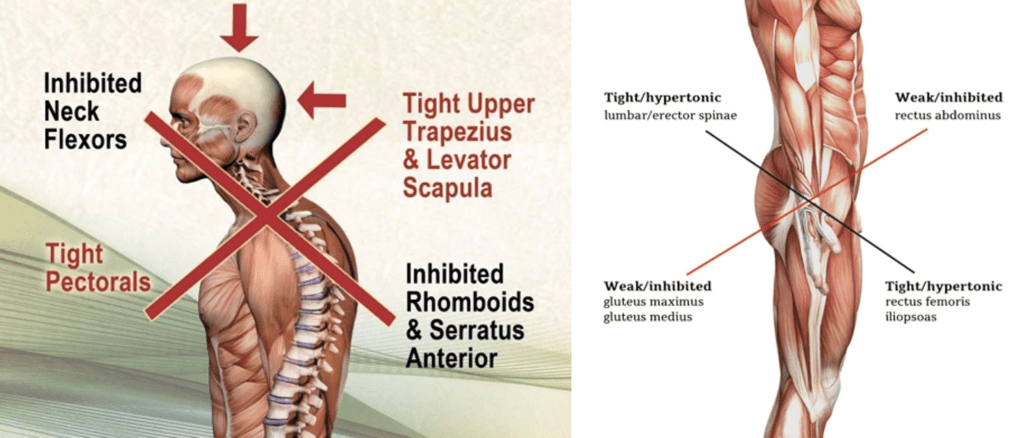
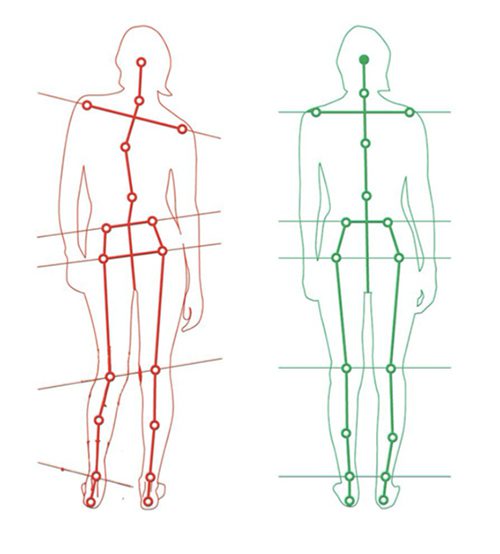
This postural assessment approach is often used to devise treatment plans by having a patient stand in front of a plumb line assessing the sagittal plane view, frontal plane view and transverse plane view, lining up bony landmarks and jotting down asymmetries on a postural chart. If a landmark fell outside of a symmetrical line it was labelled as ‘dysfunctional’ and it then needed to be rubbed with ‘lengthening techniques’ or stretched out and the opposing muscles needed to be strengthened using ‘corrective exercises’. This was further combined with multiple postural correction cues such as – position your weight over your midfoot, stand with your feet shoulder width apart, keep your knees slightly unlocked, adjust your pelvic tilt by 4.2 degrees, lift your sternum away from your pubic bone by 3 cm, retract your left scapula, retract your chin etc – and now try to walk without looking like you have a stick up your a%#@
Seems simple right?!
And your patient asks will this fix my pain?
Well, it will keep you occupied for a little while but there is little evidence to suggest that posture is causative of pain, therefore if it’s not causative then it is unlikely to curative.
So why do we focus posture so much?
We are all human, but we are not all the same. How can there possibly be a perfect posture for everyone. It’s like fitting a square peg into a round hole.
Let me tell you a few reasons why using a postural assessment for pain is unreliable.
1️⃣ There is no agreement among health professional about what is an ideal posture is
2️⃣ You have no baseline of what a normal posture for that person is before the onset of symptoms
3️⃣ People with ‘good postures’ also suffer from chronic pain
4️⃣ People with ‘poor postures’ can be completely pain free
5️⃣ Asymmetries are common and normal
6️⃣ There is no reliable way to assess posture – If you are thinking – but I can accurately palpate and eyeball the level of someone’s ASIS and assess if they have an anterior tilt, an up slip, down slip, pelvic rotation, leg length difference etc, I can also assess to see if their sacrum is rotated… well unfortunately, that is not reliable or accurate
7️⃣ There are significant differences in bony morphology. Therefore, different people have different shaped bones. And that is completely normal and common.
Let me give you some key research findings:
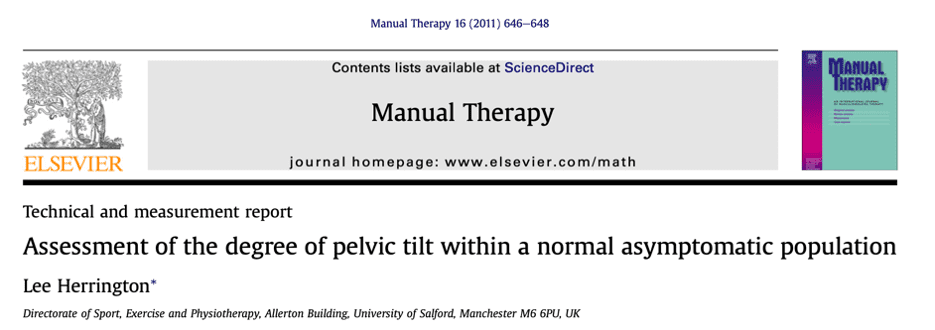
This study demonstrated that pelvic rotation and asymmetry are completely normal and very common in asymptomatic populations, In fact, they are far more common than “anatomical neutral”.
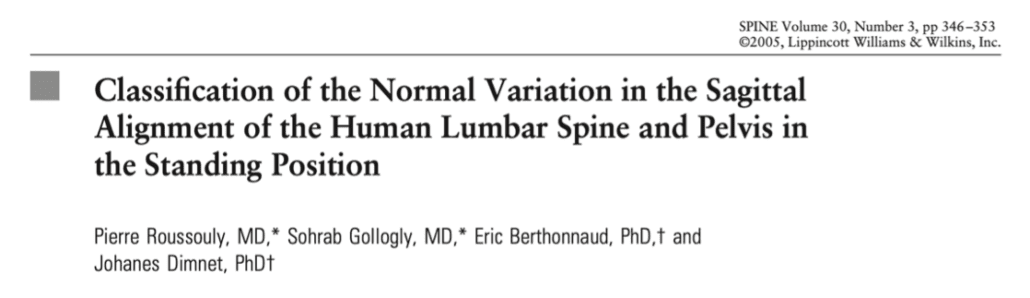
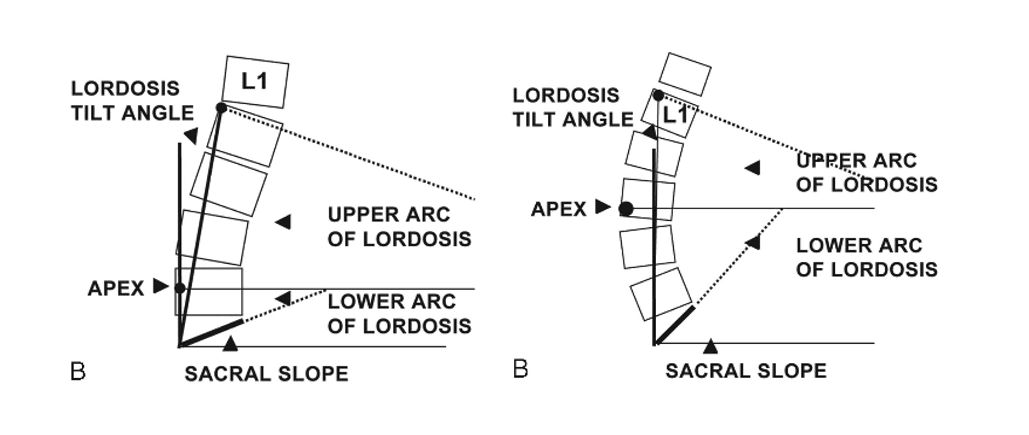
hey also found that the angle of global lumbar lordosis varied between 41° and 82°.
Interestingly the number of vertebral bodies in a lordotic orientation varied from 1 to 8.
This data suggests that the widely accepted generalization that the spine is kyphotic between T1 and T12 and lordotic between L1 and L5 may be overly simplistic!

These are normal bony variations… labelling this as postural dysfunction because it doesn’t fit ‘the norm’ is unhelpful. So, I ask you this…
Do we really need to change posture, based on a postural assessment or ‘misalignment’?
Preece (2008) has demonstrated variations in pelvic morphology with differences in ASIS height to PSIS height varying from 0 degrees to 23 degrees.
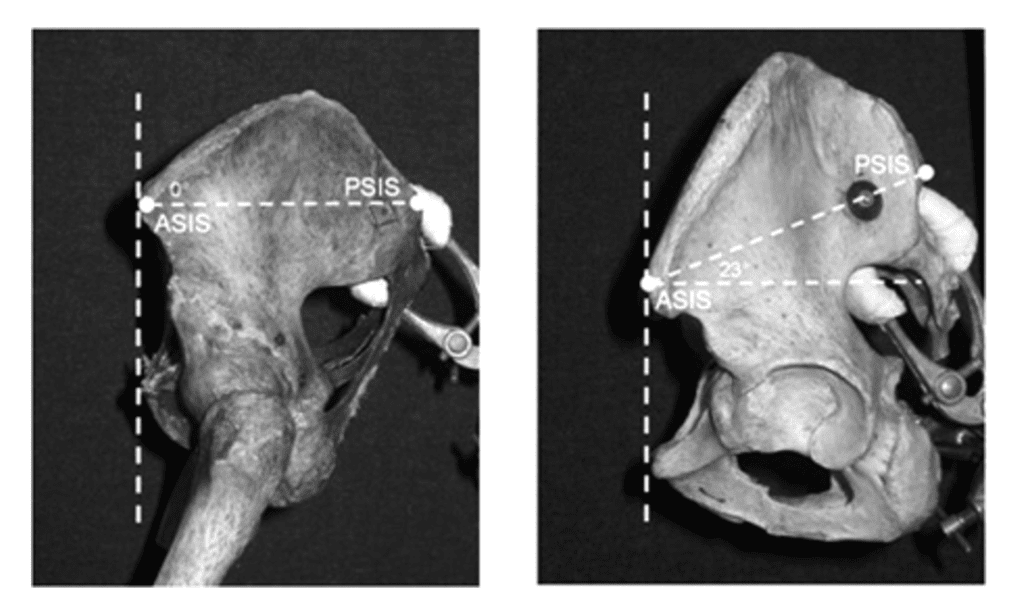
So that “anterior tilt may not be so anterior afterall? And no matter how much release work you do to psoas, it won’t change bony morphology.
You might say, I have exceptional palpation skills and can clearly see when someone is out of alignment…
If patients don’t know what an optimal posture is, then surely health professionals and physios do?
If we can’t agree on an optimal posture (if there is such a thing) and there is no reliable way of measuring it in clinical practice, there is no reliable evidence linking it to be causative of pain, then what is it that we are looking to “correct”.
We all look different on the outside, so why do we assume that that everyone’s bony landmarks should be in the same place on the inside?
Now I’m not saying that posture is completely irrelevant, but what I am saying is assessing a person’s posture, pointing out discrepancies and devising a treatment plan based on the location of structural landmarks and labelling posture to be causative of pain is inaccurate, unreliable and can be harmful to a patient’s beliefs.
Different postures matter, encourage people to move into all sorts of different positions regularly.





