TMJ in clinical practice – Part 2
Welcome back to this series on the TMJ in clinical practice.
My goal in this series is to introduce you to different factors in the assessment and treatment of TMJ related pain.
Today I’d like to bring your awareness to the temporomandibular joint (TMJ) disc.
Just like the discs in our spine, this disc exists to absorb pressure, create space and to protect the joint surfaces of the TMJ.
Unlike the discs in our spine, the TMJ disc is a highly mobile and in fact moves into and out of the joint space each time we open our mouths.
As we can see in the image below, the disc protects the joint surfaces and has a direct muscular attachment from the superior head of the Lateral Pterygoid muscle. Below it, we see the lower head of the Lateral Pterygoid attaching to the anterior surface of the condyle of the mandible.
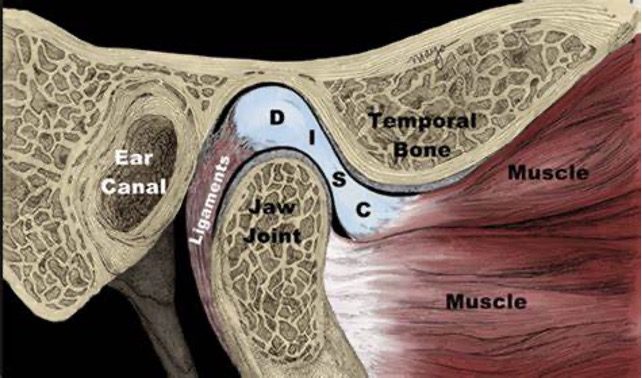
Let’s now consider what happens when the jaw opens.
We can see in the image below that the two bellies of the Lateral Pterygoid pull forward on the condyle of the mandible and the disc and translate them both anteriorly, essentially dislocating the joint itself. This occurs with each opening of the jaw.
As the condyle and disc move forward together, they help to maintain a soft tissue buffer between the articulating surface of the condyle and the lower projection of the temporal bone. This arrangement protects the bony surfaces. The disc and mandible are held in place by the ligament posteriorly.
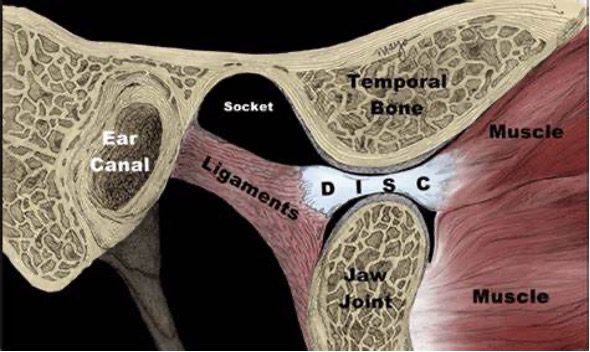
While it would be reasonable to assume that increased compression of the disc in this position might lead to pain and dysfunction, it is actually the ligament (retro-discal tissues) that sit behind the disc that are often the source of pain.
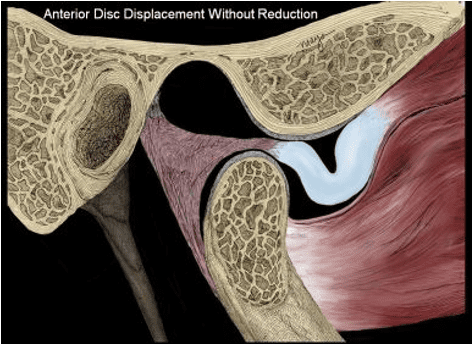
As we can see in the images below, there are two potential dysfunctional arrangements that can occur with the anatomy here.
In the first image, the jaw closes and the articulating surface of the condyle returns to its joint cavity. However, the disc is still displaced anteriorly, potentially due to a hypertonic superior head of Lateral Pterygoid not allowing the disc to return.
This causes the retro-discal tissues to be compressed and potentially result in pain.
In the second image, we see the jaw attempting to close but the mandible not fully returning to the correct position (potentially from a hypertonic lower belly of Lateral Pterygoid), resulting in the retro-discal tissues (or even the disc) getting trapped in a pincer arrangement of the condyle of the mandible and the inferior eminence of the temporal bone. It is clear to see how this could result in irritation and pain in the associated tissues.
This anterior disc displacement without reduction can also be a major barrier to full jaw opening and has often been called “Closed Lock”.
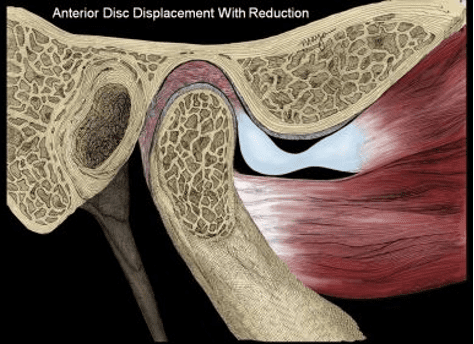
There are however other causes of disc displacement, including trauma to the jaw, or osteoarthritic changes to the joint that impact the ability of the disc to slide smoothly between the bony surfaces.
Please also keep in mind, that it is not uncommon for disc displacement to be noted on imaging/assessment, but for there to be no pain associated with it.
So this further demonstrates to us that we can never purely rely on structural mechanisms as the sole cause of someone’s pain. Often there will be other factors at play.
However, it is reasonable to consider the above described presentations as contributing factors to dysfunction and painful TMJ cases.
The main things I would like you to take away from today’s article are:
➡️ The unique anatomy design of this joint
➡️ The importance of healthy disc movement during opening and closing of the jaw
➡️ The relationship between the two heads of the Lateral Pterygoid, the TMJ disc and mandible.
➡️ The highly sensitive nature and potential for irritation of the retro-discal tissues.
The next time you assess someone’s jaw movement and palpate and listen for crepitus of this joint, consider the function of the Lateral Pterygoid and movement of the disc as part of your clinical picture.