Stop Blaming Me!
So often in clinicians and patients blame an individual muscle or structure as the cause of pain.
How often do you hear (or even say) that it’s the Piriformis, Supraspinatus or the QL…
Yes, I am sure if someone presents with pain in the buttock, shoulder or low back, these muscles may be tender to press on. However this is a huge over-simplification of pain. Lets think about what we are actually pressing on. If I have pain in my wrist, do we blame the pronator quadratus? If I have a sore abdomen, is it because of my abs? If I have a headache is it because of my upper traps? There always more to it right?
So, let’s have a look at poor little piriformis… This muscle takes a lot of the blame for buttock pain and symptoms of Sciatica. The diagnosis of piriformis syndrome is thrown around way too often, in-fact, it is outdated terminology, and it lacks a gold standard diagnostic criterion. (Fishman & Schaefer 2003; Stewart. 2003) But that’s a chat for another day!

So, in clinical practice, you come up with a diagnosis of piriformis syndrome…
I ask, how did you arrive at that diagnosis?
Well, they had buttock pain, and it was painful when I pressed on the area… (My patient also read about it on google)
I see… I have no doubt it would be sensitive to press into the deep gluteal space. Let’s take a look at the anatomy.
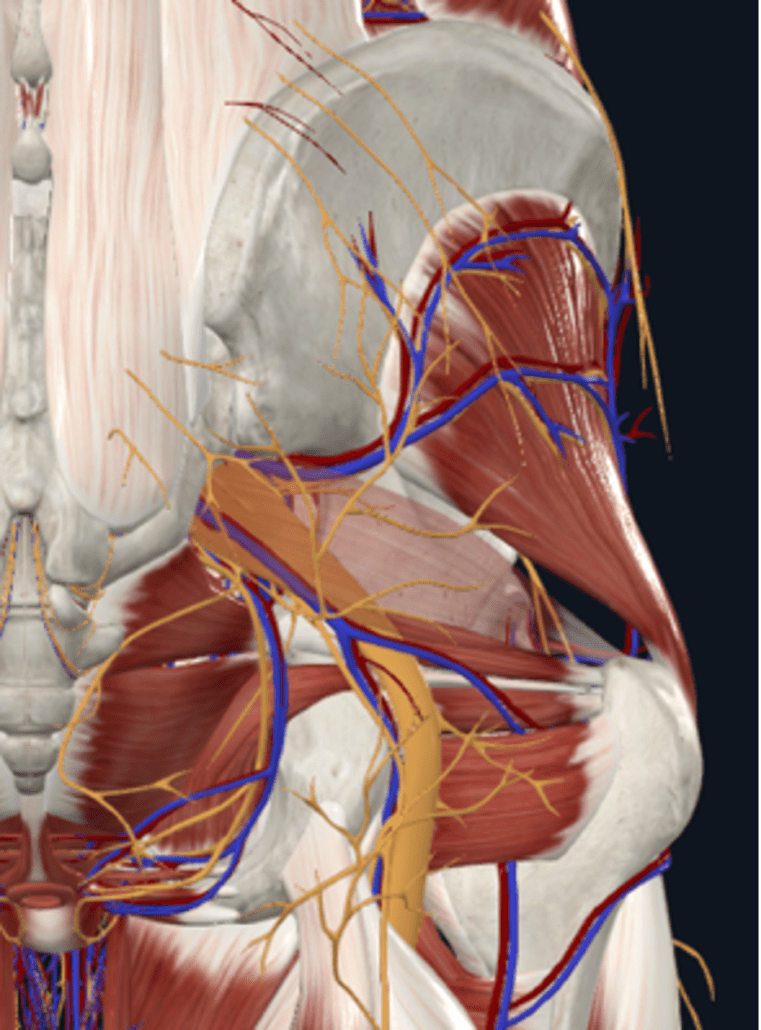
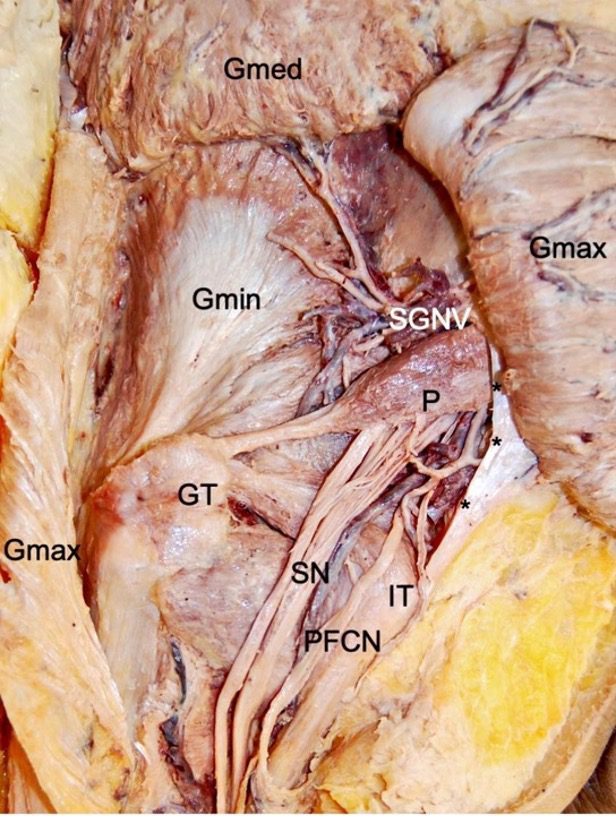
To get to the level of this muscle, we must first palpate through several centimetres of adipose tissue, several centimetres of glute max muscle and then we are in the deep gluteal space. In that deep gluteal space, there are numerous nerves and blood vessels, we then also have the hip periarticular and intra-articular structures that can be a source of buttock pain.
Can we specifically and reliable identify the nociceptive source of buttock pain with palpation?
This study by Lesher et al. found 12 different referred pain zones for hip pain with the most common being buttock pain.
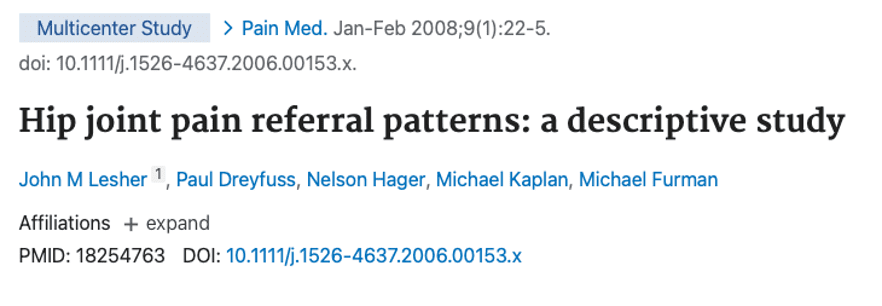
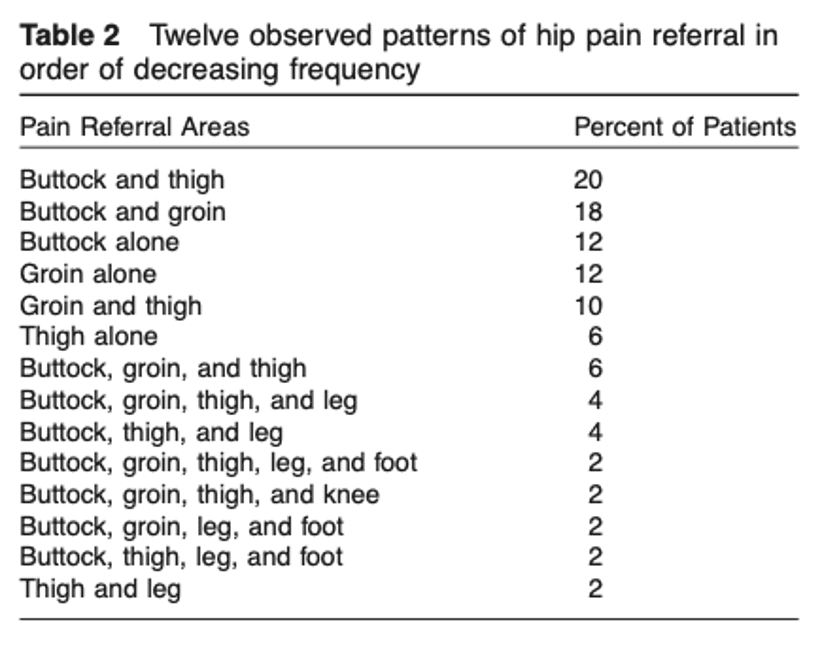
In another study by Slipman et al. (2000) examining the SIJ, 18 referred pain patterns were noted in 50 patients undergoing fluoroscopically guided SIJ injections for SIJ pain and 94% of the participants described buttock pain.

Can the piriformis be involved in buttock pain? Yes! Is it often the primary cause? Very uncommon
So, you might be thinking…What is the incidence of true piriformis syndrome?
It is between 0.3% to 6% of all cases of low back pain and/or sciatica. (Hicks BL, 2021)
You might say “But the piriformis is so close to the sciatic nerve, so I have heard it can cause sciatica…” Well every peripheral nerve in the body has a mechanical interface and various nerves will pass, under, over, around or through muscles, bones, tendons, ligaments, fascia etc.
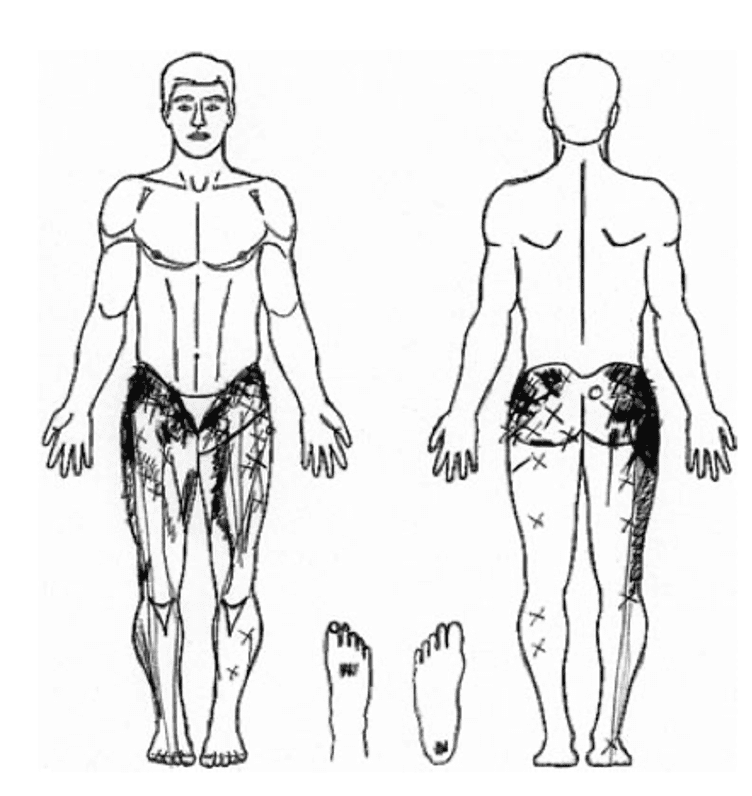
Can we accurately differentiate the Piriformis from the obturators and gemelli muscles with palpation? Take a look at the image below and you tell me?
Ok, what else could it be?
➡️ Gemellus superior & inferior, Obturator internus & externus. Quadratus femoris, Glute max?
➡️ SIJ sensitisation
➡️ Lumbar referred pain
➡️ Posterior hip impingement
➡️ Posterior labral pathology
➡️ Hip OA
➡️ Proximal hamstring syndrome
➡️ Neural sensitisation
➡️ Vascular compromise
Etc. and the list goes on.
Will driving an elbow into someone’s Piriformis be sensitive – YES! Does that mean that the piriformis is the cause of their pain? Unlikely!
Radicular pain, from nerve root sensitisation in the lumbar spine is far more common that piriformis syndrome and symptoms can often be felt in the buttock. So, if a nerve is mechanosensitive and you press in to the buttock in the location of the piriformis and the sciatic nerve, is it going to hurt?
You bet ya!
Ok, what about the QL… I hear this all the time from patients “Can you ‘release’ my QL because it’s tightening up and that’s the cause of my pain”.
Back pain is so complex and multifactorial, although the left or right side of the back may be the location of symptoms, they might not know what else is in the region and also have a biomechanical and structural view of pain… It is an over-simplistic view of the body and pain for us as clinicians to label a single muscle as the cause of pain in particularly in the absence of a specific mechanism of injury. So, what else are we pressing on when we use ischemic pressure to the QL?
Skin, Fat, Thoracolumbar fascia, Lats, Iliocostalis lumborum, Obliques, Transverse abdominus, Neurovascular structures etc.
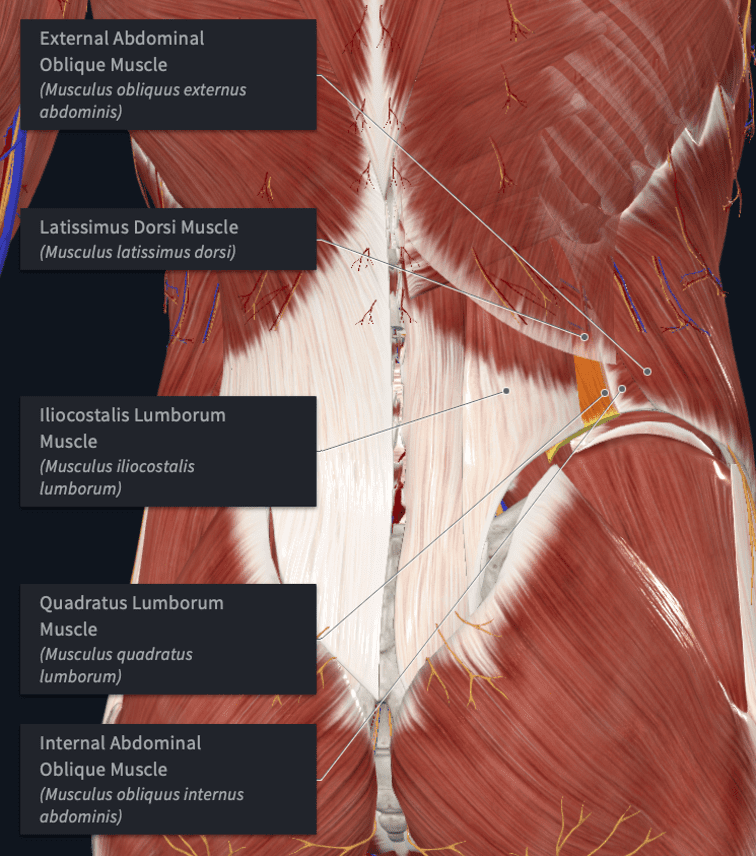
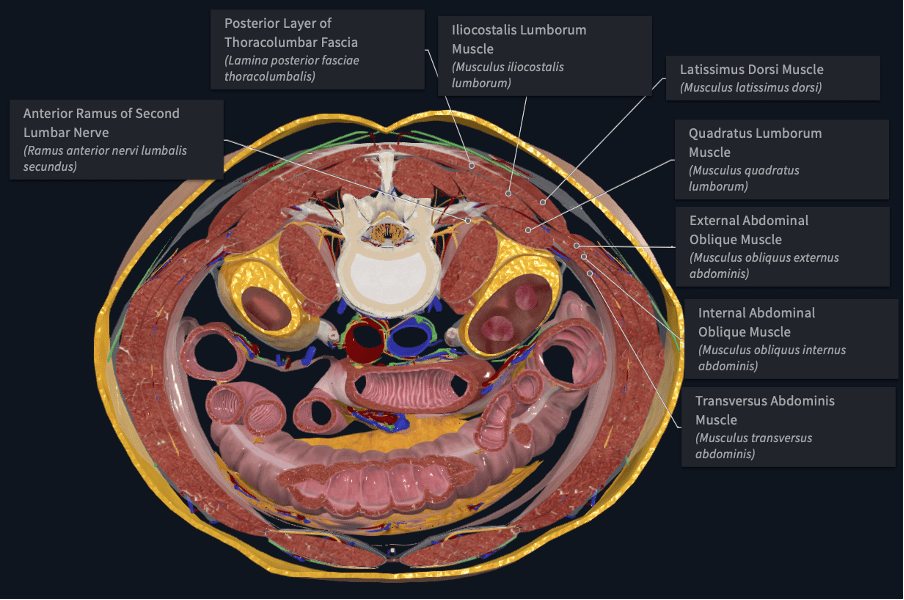
Also, you will see that the lumbar plexus is anterior to the QL.
Is their back sensitive – YES… Is the cause of their pain the QL? Well, I’ll let you have a think about that one.
It is important to look beyond isolating single muscles as the cause of pain. Yes, muscle tension and sensitivity may be a symptom and can contribute to their level of pain and irritability, however is it cause or effect? I think it is important to think a little broader about pain and manual therapy rather than labelling a single muscle as the cause.
Bodine Ledden