How much is enough?
I always get asked the question, “How much is enough?”
What I mean by this is treatment dosage.
How long should you mobilise a joint for? What grade mobilisation should I use? How long should I leave a needle in for? How much stimulation should I use? How many repetitions should I prescribe? How many times should I see a patient and the list goes on.
These are all importation variables to consider, however the focus should be on the patient and their response, not the type of intervention or technique. This is why there never will be a clear answer for dosage and nor should there be! This is because people are difference and pain is a subjective and individual experience. Looking for a one size fits all or a magical number is looking for something that isn’t there.
Everything that we do as clinicians should put our patients front and centre. The question should not be “What is the best intervention for shoulder pain?” rather “What is the best intervention for this person”?
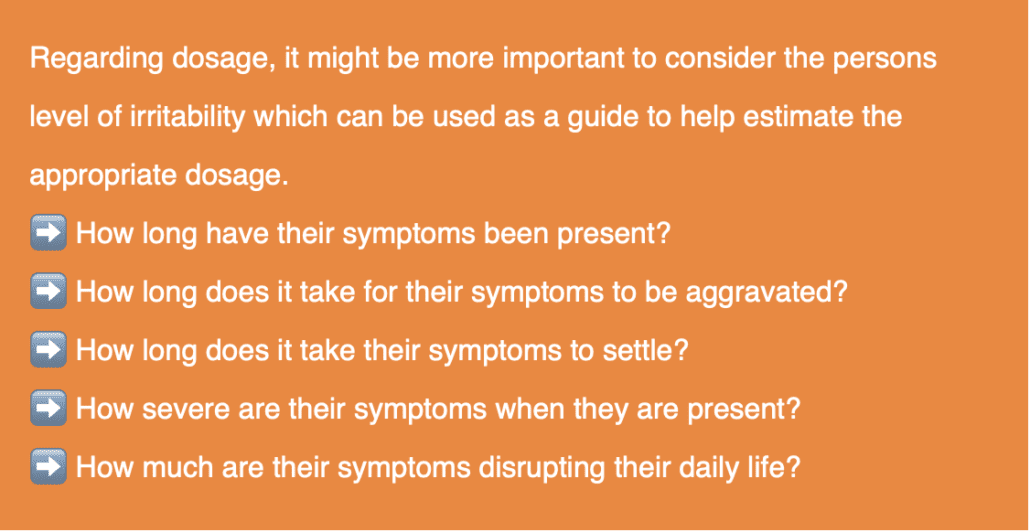
Plus considering other factors such as mood an emotional state, levels of stress etc. as these factors can significantly influence their level of irritability.
Asking these questions and gathering information about symptom behaviour can assist in getting the dosage right.
So, keep it simple…
If a patient has a HIGH level of irritability DO LESS
If a patient has a LOW level of irritability DO MORE
Then, follow them up soon after treatment to see their response.
From there you can reflect:
Do we then need to increase or decrease treatment dosage?
Do we need to increase or decrease treatment frequency?
Do we need to increase or decrease training volume?
This will ALWAYS be based on the individual patient.
If your patient “Sally” has carpal tunnel syndrome and her symptoms onset 30 minutes into using a computer at work and the symptoms are 8 out of 10 for the rest of the day, then we might categorise her as highly irritable. Therefore, a high dosage of manual therapy and getting her to do 50 neurodynamic mobilisations every hour would likely be too much for her at that point which may aggravate symptoms. It might be more appropriate to have much shorter treatment sessions, use less aggressive treatment techniques and prescribe much lower volume of movement or exercise.
However, if her symptoms onset 4 hours into her shift at a mild 3/10 and her symptoms are relieved by the time she gets home, a higher dosage might be indicated.
To get treatment dosage right, focus on the person, monitor their symptoms and level of irritability. Don’t look for a magical number, duration of time or repetitions. These factors are all variable person to person and week to week. Gain regular feedback, assess, treat, and reassess.
Our role in many cases is to modify symptoms appropriately and progressively move towards engaging our patients in more active approaches. This doesn’t need to happen in one session, so we don’t need to throw the whole kitchen sink at them, more is not necessarily better. Understand the natural course of healing and progressively over time assist our patients to get more comfortable with what was once uncomfortable.