Case study time..
Let’s tickle your dendrites, fire up your axons because this case study will get you more excited than an action potential.
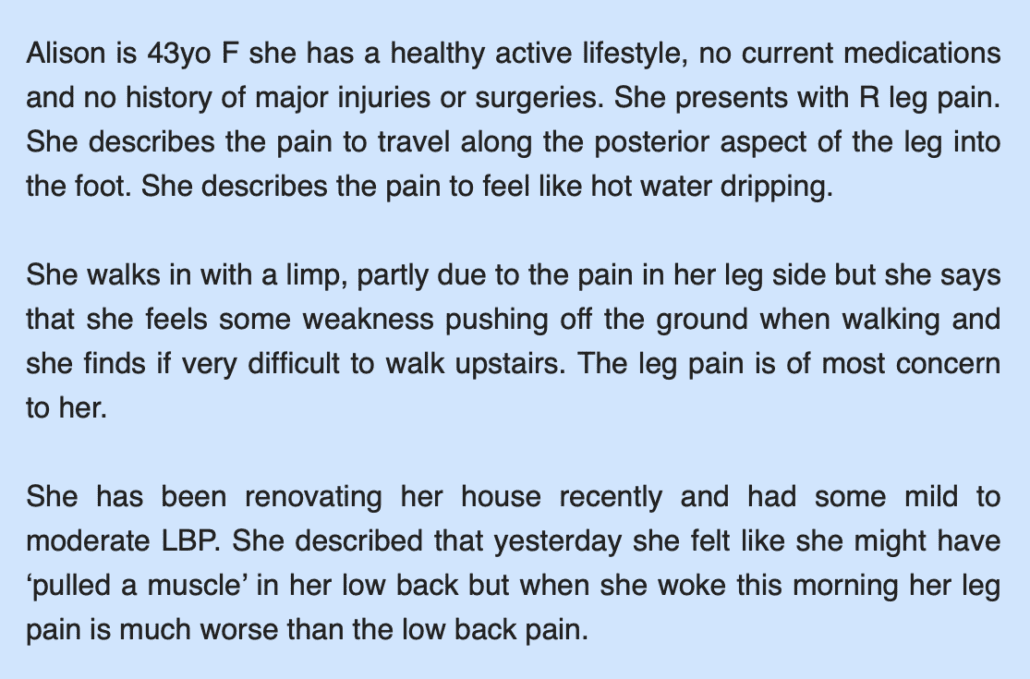
What comes to mind for you?
Does your mind go completely blank? Do you panic? Or do you get a rush of possible differential diagnosis rushing to your head?
It might be easy to point the finger are a single structure or pathology and rule it in straight away, however there is often more to the picture. (Let me also stop you from blaming the piriformis so cross that one off the list!)
Before we spill our thoughts, or even attempt any treatment we should be aiming to confirm or deny our list of potential differential diagnoses based on signs, symptoms, and clinical examination. The best way to do this is a structured process to ruling conditions out.
In the front of our mind should be a list of different possibilities that we need to sort through. Firstly, we should start off with the most serious so we can rule it out.
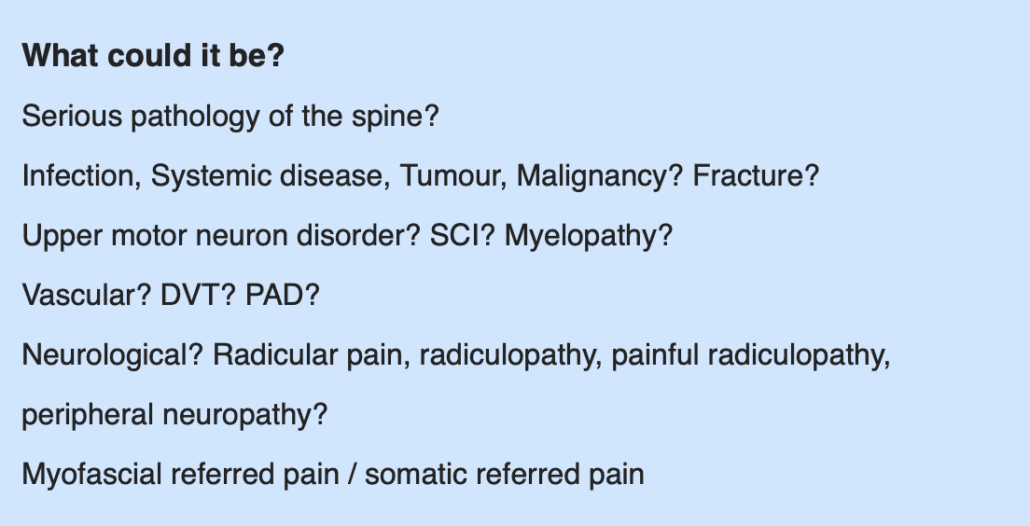
Once we have ruled out signs of serious pathology, we can process…
If neurological symptoms are present, are the symptoms nerve root related?
Or related to peripheral nerves? Is it due to an injury to the hip knee or ankle?
Are there signs of impaired nerve conductivity? Gain of function or loss of function?
Not all cases fit a clear clinical picture, it is important to approach cases like this with a thorough systematic approach to gaining medical history and performing a thorough physical examination.
So where would you start?
Do you start with the leg? Are the leg symptoms primary, or secondary. Or do we start with the spine?
➡️ Functional movements
➡️ Sensory, muscle power, reflex?
➡️ Neurodynamic assessments
➡️ Neural palpation
➡️ PA provocation of lumbar spine
The case study describes the leg pain being worse than back pain, so you could be forgiven questioning peripheral nerve involvement or muscle tear due to leg pain and weakness, however there is absence of a mechanism of injury and also with radicular pain, the leg pain is often worse than back pain and the radicular symptoms may not always onset immediately.
What does that all mean and where do we go from here?
I get it, assessment can be challenging. Interpreting that information can be even more challenging.
But based on this information understanding the key signs and symptoms may provide us with some insight into what may be going on such as:
- Neural pain (causalgia) into the leg and foot – Pain in the S1 Dermatome ➡ signs of radicular pain
- Sensory changes with sensory tests in the S1 Dermatome – Sensory gain or sensory loss
- Weakness/ diminished function pushing off when walking (plantar flexion) S1/S2 Myotome ➡ signs of impaired conductivity – Radiculopathy
- Diminished or absent Achilles tendon reflex (S1/S2) ➡ Signs of altered conductivity / conduction block
Pain with Straight leg raise (SLR) ➡ agg with dorsi flexion ➡ Sciatic nerve mechanosensitivity
While none of these tests are highly useful in isolation, clustering them together can improve the accuracy and diagnostic utility.
Allison’s symptoms on subjective examination provide us with clues to look for a neurological deficit and based on these symptoms we can apply a clinical examination to confirm or deny our diagnosis. In this case, signs, symptoms, and clinical examination are consistent with a S1 painful radiculopathy.
Yes, this can sounds quite scary, but prognosis can be very good in a lot of cases. You, as a manual therapist will at some point (if not already) be presented with a case like this. Having the skills to assess can help you to differentiate neural pain disorders from musculoskeletal pain disorders, rule out red flags and serious patholgy with greater certainty and either write a through referral or direct the appropriate rehabilitation plan.
And while cases don’t always fit a perfect clinical picture, performing a structured clinical examination in combination with signs and symptoms can provide direction towards appropriate management. The assessment process can assist in avoiding unnecessary imaging, injections and surgery.
This case has some stand out features however many cases that present to us in clinical practice may not stand out so easily and we need to dive a bit deeper in our examination. In some cases, the neural component can be overlooked and missed.
I would love you hear your thoughts on this or other neural pain presentation cases that you have seen. Any challenges, success stories or questions. Let me know! 🙂
Bodine Ledden