The hand anatomy mini-series – Connective tissue
The skeletal anatomy of the hand was covered in one of our recent blogs which you can read or review now with the link, here. Covering the connective tissue of the hand, we’ll see how the numerous joints are supported whilst still allowing for the large range of motion needed for our daily activities.
Each joint of the hand has its own articular capsule, forming a synovial joint. The articular capsules themselves provide support and limit excessive movement between articular surfaces. This is then further strengthened by ligamentous tissue, some of which, blends with the articular capsules directly.
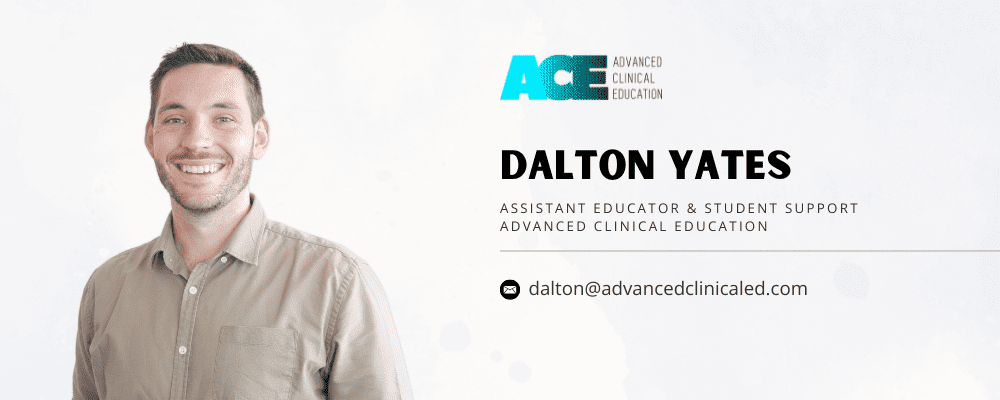
The palmar carpal ligament and extensor retinaculum of the wrist form a continuous fibrous band which functions to hold tendons of the wrist and hand in place. These two structures cover numerous tendonous sheaths, which are shown in figure 2 (anterior) and 3 (posterior).
These tendinous sheaths compose of an outer fibrous sheath, and inner synovial membrane, providing a thin layer of lubricating fluid for a smooth surface to reduce friction of the tendons during movements.
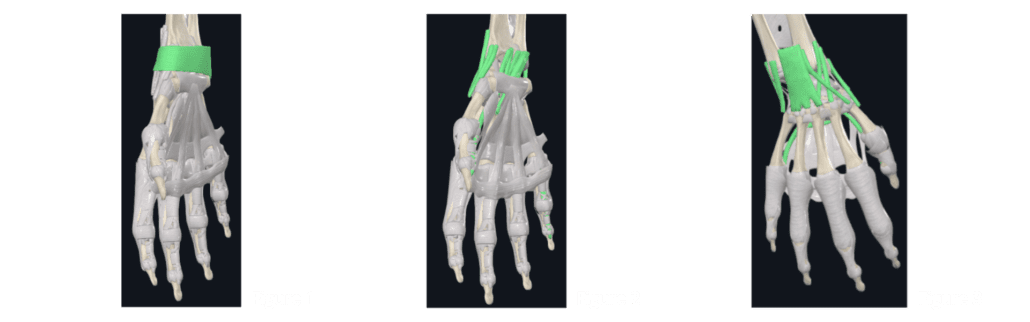
Figure 4 highlights the palmar radiocarpal ligament complex. This comprises of the radioscaphocapitate ligament, the long and short radiolunate ligaments (2 and 3), and the radioscapholunate ligament (4) which is posterior to the long radiolunate ligament. This ligament complex strengthens the articular capsule of the radiocarpal joint.

The last two ligaments of the radiocarpal joint are the radial collateral ligament (figure 5), and the dorsal radiocarpal ligament (figure 6). Again, these both function to strengthen the articular capsule of the radiocarpal joint.

The ulnar does not articulate with the carpal bones. However, there are several ligaments that insert from the ulnar to the carpals. Like the palmar radiocarpal ligament, this divides into individual parts; the ulnolunate ligament (1), the ulnocapitate ligament (2), and the ulnotriquetral ligament (3).
The ulnar collateral ligament (figure 8), again, thickens the articular capsule of the wrist, originating from the ulnar styloid process and inserting onto the triquetrum. This is also true for the dorsal ulnocarpal ligament (figure 9).

The palmar aponeurosis (figure 10) is made of both longitudinal and transverse fibres which provide both an insertion (palmaris longus) and an origin (palmaris brevis) point for muscles. Consisting of superficial, intermediate, and deep layers which attach to the skin of the hand as well as bone, this helps to improve grip whilst also protecting underlying structures.
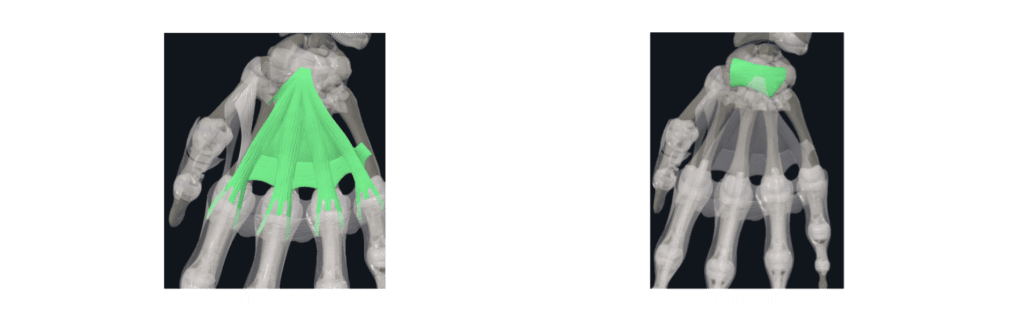
Forming the roof of the carpal tunnel is the flexor retinaculum (figure 11) of the wrist. The structures that pass through the carpal tunnel are the flexor digitorum profundus, flexor digitorum superficialis, flexor pollicis longus, flexor carpi radialis and the median nerve.
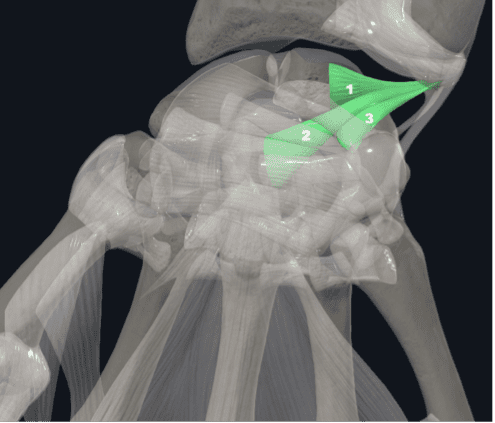
Preventing separation of the webbed space between the thumb and index finger are the proximal and distal commissural ligaments (figure 12). The proximal ligament is an extension of the transverse fibres of the palmar aponeurosis, whilst the distal ligament extends from the superficial transverse metacarpal ligament (figure 13). Similarly, the superficial transverse metacarpal ligament functions to reduce the movement of the carpometacarpal and intermetacarpal joints.

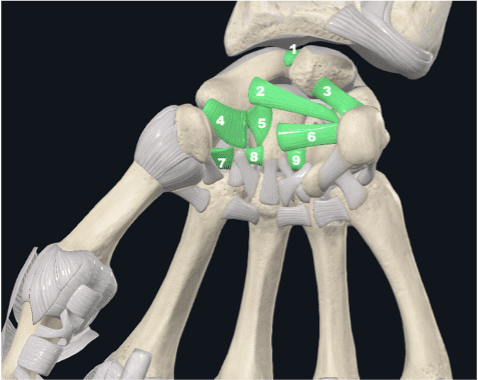
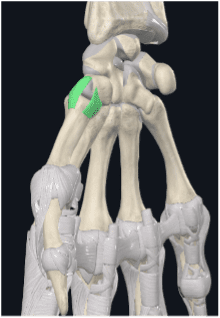
Forming the palmar intercarpal ligament complex are 9 individual ligaments. These are listed and shown in figure 14 – scapholunate interosseus ligament (1), palmar lunotriquetral ligament (2), scaphotriquetral ligament (3), scaphotrapeziotrapezoidal ligament (4), scaphocapitate ligament (5), triquetrocapitate ligament (6), trapeziotrapezoidal ligament (7), palmar trapezoideocapitate ligament (8), and palmar capitohamate ligament (9).
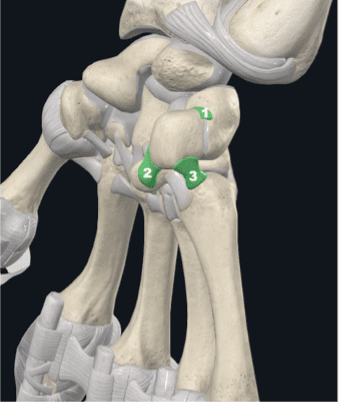
To stabilise the pisiform, the pisotriquetral ligament (1), pisohamate ligament (2), and the pisometacarpal ligament (3), form the ligamentous complex of the pisotriquetral joint.
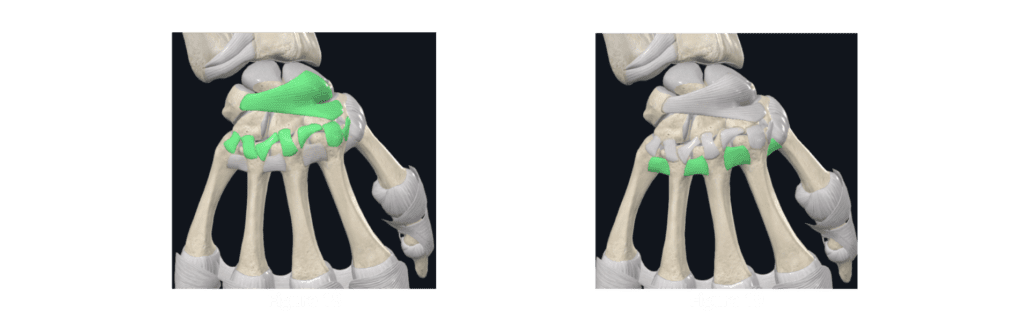
Supporting the carpometacarpal joints are two series of ligaments; the palmar carpometacarpal ligaments (figure 16) and the palmar metacarpal ligaments (figure 17).
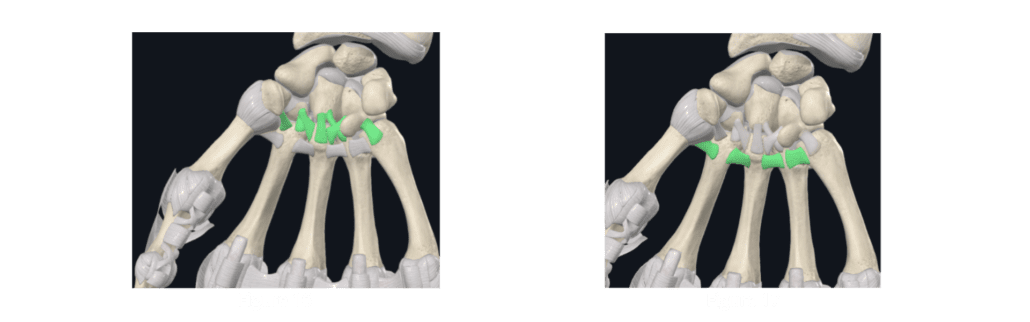
These are accompanied by the large dorsal intercarpal ligament and the seven dorsal carpometacarpal ligaments shown in figure 18, as well as the four dorsal metacarpal ligaments (figure 19). These further support the carpal and carpometacarpal joints, limiting excessive movement whilst allowing for the gliding articulation between joints.
The thumb is supported at the first carpometacarpal joint by the lateral carpometacarpal and the palmar carpometacarpal ligaments. These originate from the trapezium and insert onto the first metacarpal, the thumb.
The last of the connective tissue supporting the hand dorsally are three structures; the extensor hood (proximal) and the triangular ligaments of the finger (distal), shown in figure 21. The extensor hood provides an insertion site for intrinsic muscles of the hand, whilst the triangular ligaments of the fingers prevent separation and anterior displacement of the lateral digital sheaths shown in figure 22 during flexion.
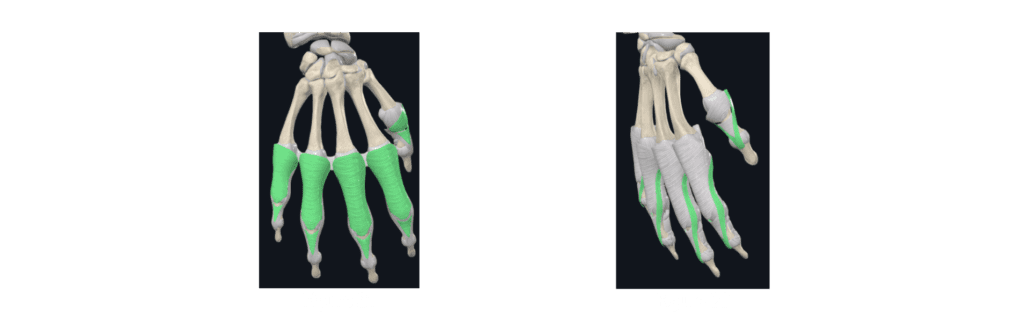
Providing support to the metacarpophalangeal joints are three broad fibrous bands, the deep transverse metacarpal ligaments. Like the superficial transverse metacarpal ligament from figure 13, these further assist in limiting excessive movement of the metacarpals.
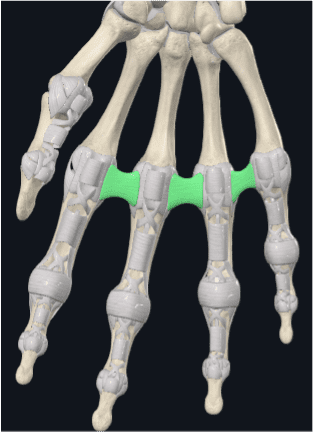
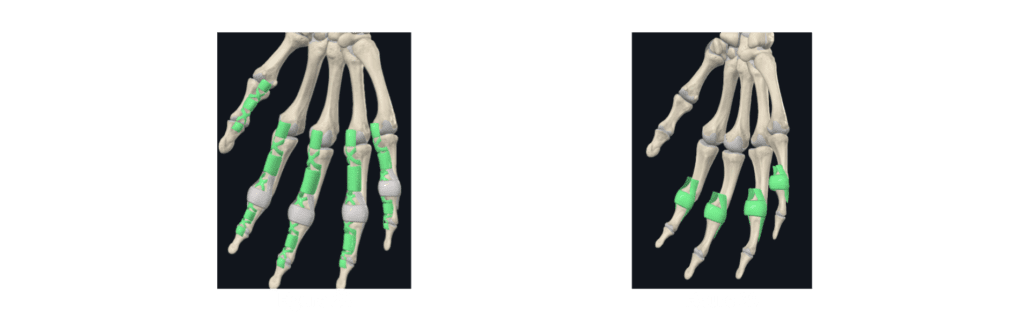
Each of the metacarpophalangeal joints are supported by their primary stabilising ligaments; the proper collateral metacarpophalangeal ligaments and the smaller accessory collateral metacarpophalangeal ligaments (figure 24) that sit proximally to these. Acting to increase the surface area for articulation of the metacarpal head is the palmar metacarpophalangeal ligaments (figure 25), whilst further supporting the metacarpophalangeal joints.

The proximal and distal interphalangeal joints are supported by their respective collateral and accessory collateral ligaments (figure 26) and palmar ligaments (figure 27), likewise to the metacarpophalangeal joints.
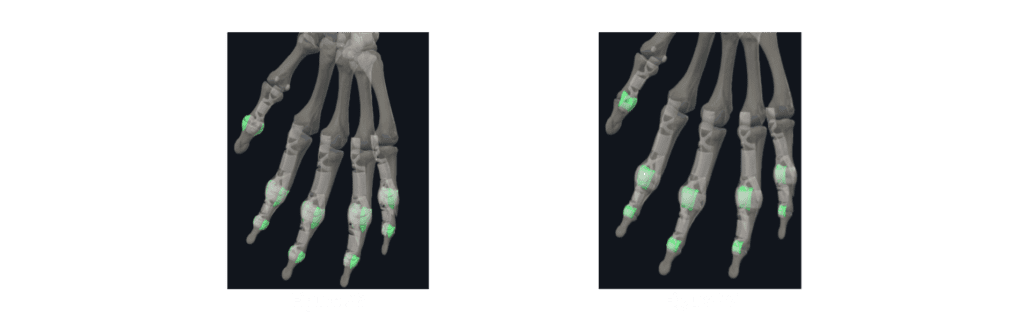
The final connective tissue structures that support the hand are the annular and cruciform parts of the fibrous sheath of the digits of the hand (figure 28), and the transverse and oblique retinacular ligaments (figure 29). The annular and cruciform parts of the fibrous sheath both function to reduce ‘bowstringing’ of tendons of the palmar surface of the hand, whilst the transverse and oblique retinacular ligaments stabilise both the interphalangeal joints and the extensor apparatus (the muscles/tendons and connective tissue that function to extend the digits).
The next part of the hand anatomy mini-series will be covering the muscular anatomy of the region, continuing to build upon the foundations that we’ve covered for the anatomy of the hand.