6 Myths about sacroiliac joint pain
Myth #1 The SIJ can become unstable
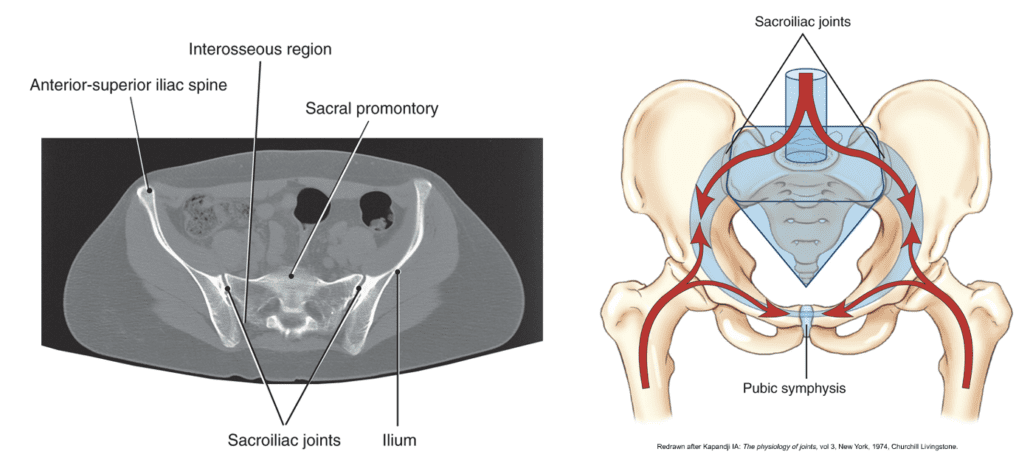
The SIJ functions to provide stability and the transmission and dissipation of load from the trunk to the lower extremities. (Thawrani, 2019) The SIJ is an inherently stable structure with only a small 6 degrees of movement available during normal activity. (Palsson et al. 2019)
During development the SIJ changes structure, it changes from a synovial joint to a synarthrodial joint where it allows minimal to no movement. The articular surfaces change from smooth to rough after puberty. The stiffening of the joint is to increase the resistance against movement and vertical shear force between joint surfaces. Therefore throughout adulthood, the joint becomes increasingly fibrotic and less mobile.
The SIJ does not become unstable or ‘go out of place’ as we get older, it actually gets stiffer and less mobile.
Myth #2 The SIJ becomes unstable after child birth

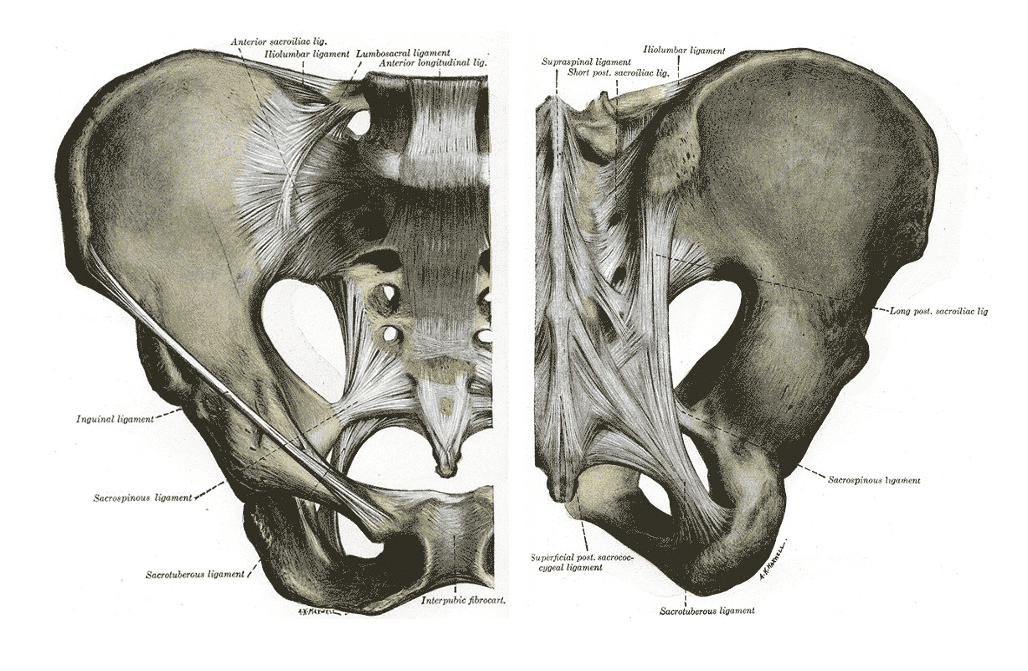
SIJ pain is more common in pregnant women. A significant increase in joint laxity occurs during the last trimester. The combination of weight gain, hormonal induced joint laxity may sensitize SI ligaments and joint capsule and therefore the SIJ can be a source of nociception however this is not linked to structural instability.
The influence of this perception can instill fragility, hypervigilance, excessive muscle guarding and lead to avoidance and other psychological and behavioral changes.
SIJ pain and sensitisation should be considered in the multifactorial nature of pain including the change in lifestyle, stress, mood, emotions, sleep, environment, changes to activity, beliefs, support network, hormonal and various other biological changes associated rather than joint instability.
It is sensitized… not unstable.
Myth #3 You can accurately assess sacroiliac movement
Some clinicians believe they can detect the amount of movement that occurs at the SIJ and accurately palpate the exact position of the sacrum that is therefore linked with pain.

Test such as stork test, sitting flexion test, standing flexion test, prone knee flexion test and SLR have been shown to be impossible to detect the amount of SIJ movement.
SIJ movement test do not have any diagnostic value. These tests are unreliable and have poor clinical utility (Hungerford, B.A., 2007)
Perception of movement could be attributable to other factors such as soft tissue motion or pain-associated muscle activation as a response to nociceptive activity (Palsson et al. 2019)
This is important to understand as a clinician. By performing these tests and then telling the patient that there is a biomechanical dysfunction that is causing their pain is just not accurate and this can affect patients’ interpretation and beliefs about their pain which can influence their behaviors and ultimately negatively influence long-term outcomes.
Myth #4 SIJ movement dysfunctions and altered pathomechanics cause SIJ pain
Often clinicians will link movement dysfunctions to the cause of SIJ pain.
There is no causal relationship between any movement dysfunction and pain that can be identified. Movement dysfunctions such as asymmetry, instability, positional faults, torsions, upslips, downslips, inflares, outflares are inaccurately labeled as causative.
An association between movement dysfunction and pain should not be mistaken for causality. (Palsson, S et al. 2019)
Pathoanatomical explanatory models such as structural weakness, abnormality, or instability can undermine a person’s perception of the reversibility of symptoms and promote movement-related fear. (Palsson, et al 2019).
Using a pathoanatomical model to describe SIJ pain is often far too simplistic and does not encompass the multifactorial nature of pain.
Myth #5 Poor posture and misalignment causes SIJ pain
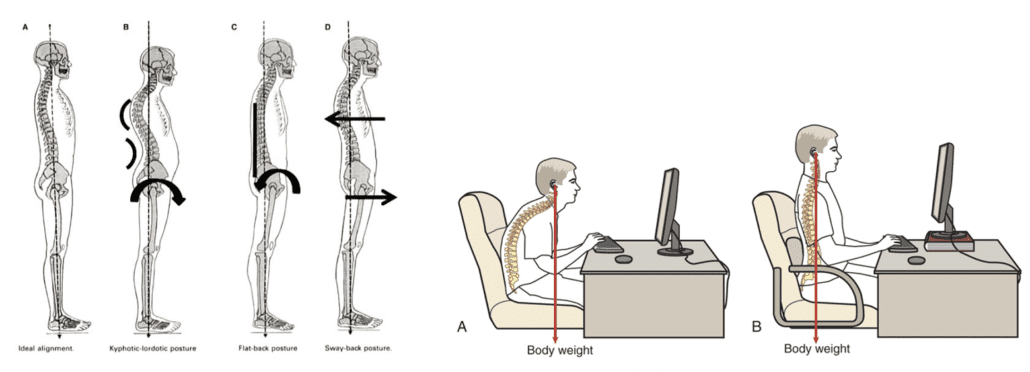
Common beliefs of spinal asymmetry, lumbopelvic and sacroiliac postures leading to pain through adverse loading and applying excess stress to the SIJ however this this has not been demonstrated in the literature with no links to pelvic positions/postures correlating to pain. (Brukner & Khan. 2017)
There is uncertainty around the SIJ as a source of pain and therefore debate about what the best management approaches are this is often due to there often being no know mechanism of injury in most cases.
Myth #6 Pain provocation tests can provide an accurate diagnosis of SIJ pathology
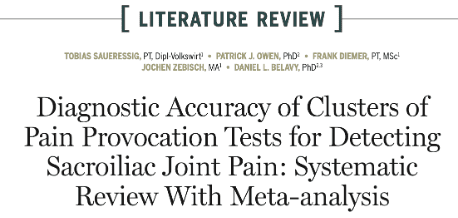
Pain provocation testing can indicate increased sensitivity of the tissues, However they cannot specifically tell us the structure causing the pain or that movement dysfunction is associated with pain (Juch et al. 2017)

Clustering pain provocation tests can be useful to rule the SIJ ‘OUT’ as a source of pain but cannot be used to rule the SIJ ‘IN’.
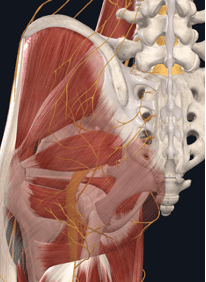
It is difficult to get an accurate diagnosis of SIJ pain due the complex anatomy and the interplay between connective tissues, ligaments muscles, nerves and joints and therefore the Specific source of nociception if often hard to identify.





