The hand anatomy mini-series
The hand is usually seen as quite a complex area of the body. It can be difficult to treat as there are so many overlying structures, it might be hard to know what you’re assessing or treating, let alone doing this with accuracy and precision. So, it might be best to get our hands dirty and grasp a better anatomical understanding of the hands over an anatomy mini-series!
We’ll first start by looking at the skeletal anatomy. Our digits are numbered from one to five – one being the thumb, and five being the pinky or small finger. They each comprise of various phalanx bones. We have five distal phalanges, one for each digit –
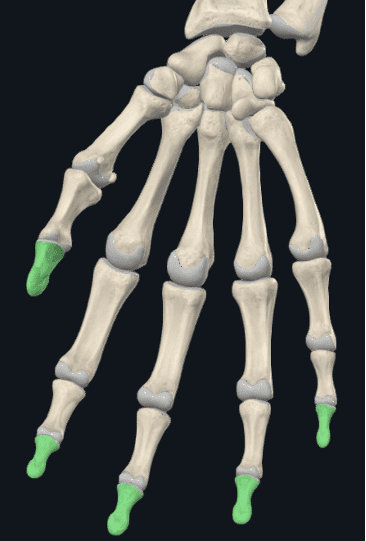
Moving proximally, we have four middle phalanx bones. Notably, we do not have a middle phalanx for the first digit, only for digits 2-4 –

We then again, have five proximal phalanx bones, highlighted below on the left image. These articulate superiorly with the first to fifth metacarpals respectively. You can see that the superior phalanx of the first digit articulates directly with the distal phalanx, having no middle phalanx between them –

Those with an attention to detail may notice two small bones over the distal aspect of the first metacarpal that aren’t highlighted on the image to the right. These are the lateral and medial sesamoid bones, found within the tendon of the flexor pollicis brevis and adductor pollicis respectively. Like the patellar, these help to align the direction of force of these muscles, as well as reducing friction and increasing mechanical advantage.
When assessing or noting the joints of the digits, we label these by being the left or right hand of course, as well as which digit is being assessed. The first digit only has one interphalangeal (IP) joint, between the distal and proximal phalanx. For digits two to four, we have a distal interphalangeal (DIP) joint, and a proximal interphalangeal (PIP) joint. For all digits, we also have a metacarpophalangeal (MCP) joint.
So, if making notes on this, it may look something like: Px w/ AROM flex at first IP and second MCP joints.
Continuing on, we have more difficulty to remember each of the carpal bones proximal to the metacarpals.
There are a few mnemonics to help remember the names and their order. You may have heard that Sally Left The Party To Take Cathy Home, and I’ll let you Google the other common one as to what happens after the party.
Here, the bones are numbered to help with putting their name and position along with the mnemonics –


1. Scaphoid
2. Lunate
3. Triquetrum (posterior to the Pisiform bone)
4. Pisiform (anterior to the triquetrum)
5. Trapezium
6. Trapezoid
7. Capitate
8. Hamate
As you could see in the images, the joints and articular surfaces of the carpals are much more complex than most other joints. A large portion of the carpal bones surface areas are taken up by articular surfaces.
It is only the scaphoid and lunate that articulate with the forearm at the radiocarpal joint. This along with the size and location of the scaphoid bone has it most susceptible of the carpal bones to fracture in a FOOSH injury. And importantly, due to the limited blood supply, it is also quite susceptible to avascular necrosis following fracture.
According to Aitken and Court-Brown (2008), thankfully, the carpal bones are least likely to fracture in the hand, at 12.2% of 1430 hand fractures recorded. The metacarpals and phalanges were at 33.8% and 54.1% respectively.
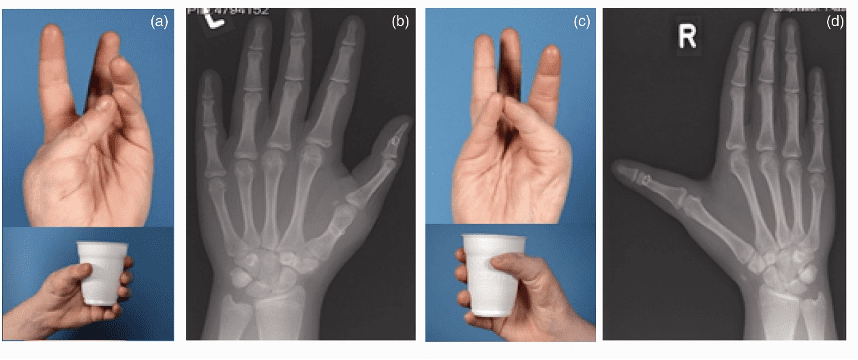
There are several anatomical variations we may see in the hand. Very interestingly, triphalangeal thumbs are a very rare anatomical variation, occurring in 1-in-25,000 births, mostly hereditarily. You can see a case below where the right thumb has a middle phalanx –
More common and predominantly asymptomatic, there are many variations in the carpal physiology. This has varying reports from an incidence of accessory carpal bones in 1-4%, and as high as 11.5% of cadavers as reported by Alemohammad et al. (2009).
Senecal et al. (2007), claimed that the four most common are the os centrale carpi, the os radiale externum, the os triangulare, and the styloideum bone.
Similarly, it’s also common for ossification to occur between two or more of the carpal bones, reducing the number of individual carpals in the hand. Again, this is reported vastly as asymptomatic in individuals, presenting most commonly with forced physical efforts with extension of the wrist and hand.
These are an important consideration, as whilst they mostly present asymptomatically for individuals, their presence and structure may be a consideration in painful presentations.
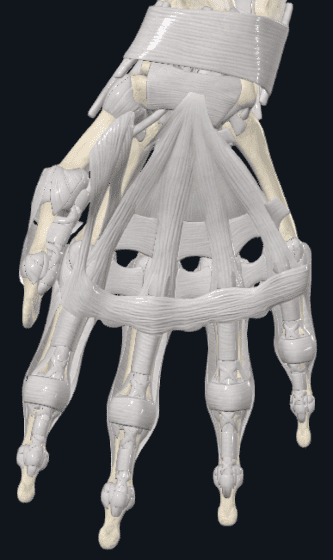
In the next blog of this series, we’ll overlay the immense connective tissue structures of the hand to better understand the pathoanatomy of this area –