Are you focusing on the wrong thing?
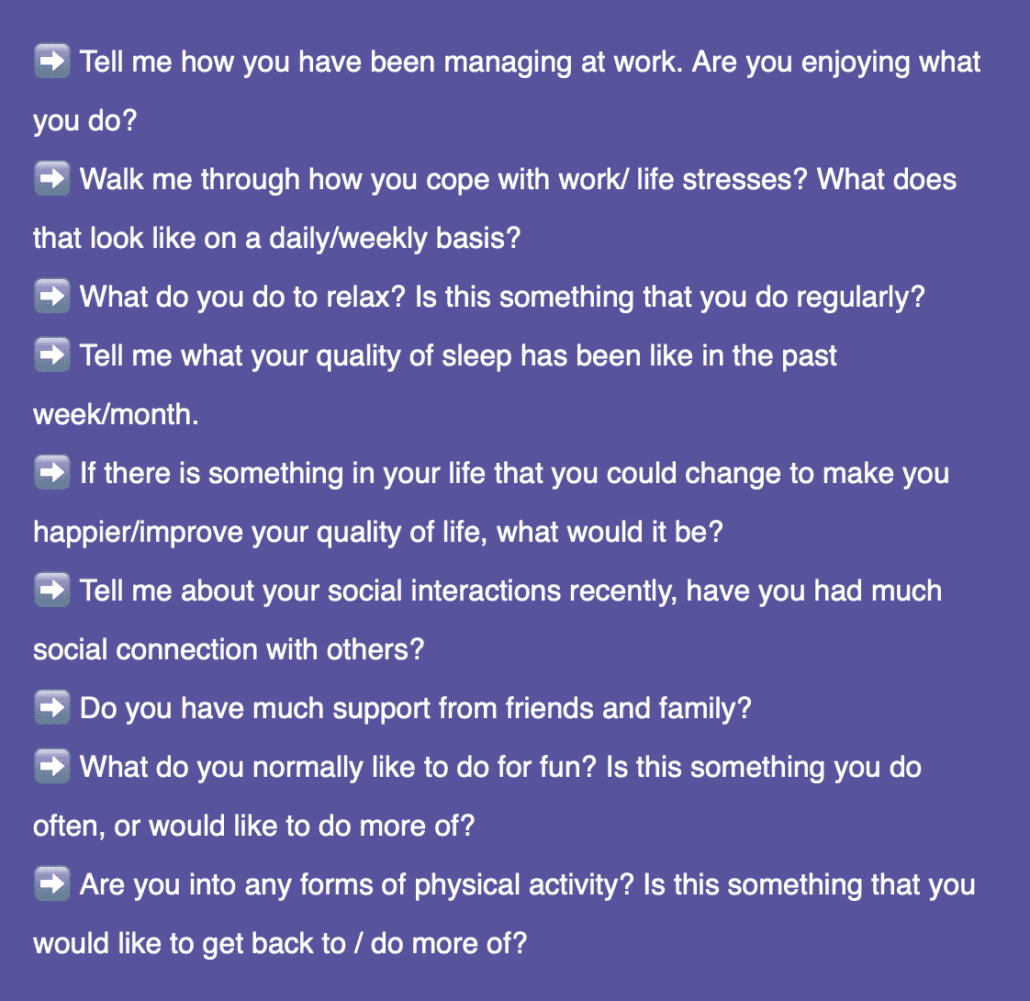
Do you ask questions like, how is your pain today? How has your pain been over the last week? What is the level of pain you are feeling at the moment? Tell me more about your pain…
Directing attentional focus to the pain may not be helpful. Now don’t get me wrong, I know pain may be the underlying reason that that patients come to see you and it is important, but the experience of pain is complex.
Remember that pain is a subjective and conscious experience, and we can often see pain in the absence of tissue damage (yes that’s right, not all pain is due to nociception). By repeatedly directing attention to pain and structure can reinforce the belief that there is something damaged/broken and needs fixing with a manual intervention. This repeated attention can also lead to ‘ownership’ of pain.
Could we ask better questions by focusing on the person and the other behavioural, psychological, social and lifestyle factors?
Try to replace the word ‘pain’ with ‘sensitivity’. Then we can talk about things that can influence sensitivity.
It is a common belief that pain is the cause of why someone has a poor quality of life, and it is the pain that has caused a cascade of events after the onset of pain and therefore all intervention is directed at treating ‘the pain’.
Consider this… What if pain is a manifestation of physiological, psychological, emotional, and social factors and the summation of these factors over time influenced the experience of pain. If these factors can be modified, will that change the persons level of sensitivity without affecting structure or mechanics of the body?
In this perspective, pain is the symptom… Just treating symptoms will not resolve the cause.
If we are only focusing on mechanical causes and painful structures, then that implies that a mechanical intervention would “fix” the problem. Unfortunately, this is not what is seen in persistent pain, and as we know, pain is a construct of multiple factors.
If we can shift the attentional focus away from structure, it is an opportunity to address other contributors, that can aid in improving coping strategies and build our patient’s self-efficacy. By doing this we can start setting goals with our patients that can assist in improving their quality of life.
Perhaps it is this improvement in quality of life that can reduce pain and not the contrary.
Give it a try I am interested to see how you go. Let me know!