I can feel how tight it is.. Can you?
Palpation is a valuable tool that can aid building our therapeutic alliance and support our assessment and treatment approach. It allows us to search for areas of pain and confirm these areas of discomfort with our patient. In manual therapy, we are trained to feel for tight muscles, taut bands, tender spots, with the belief that these findings provide a reason for a person’s pain, and there may be some merit to this approach. But how reliable is palpation of tissue to guide clinical decision making?

A common clinical assumption is that a “tight” or “stiff” muscle must be pathological. We know that there is a poor correlation between pain and tissue pathology, so is this also true for muscle stiffness and tonicity? In an observational study, Rabelo et al. (2023) investigated myofascial stiffness in individuals with plantar fasciopathy. To assess for myofascial stiffness objectively, an indentometer was used. The results found that when comparing the symptomatic side to the asymptomatic side, the symptomatic side had reduced stiffness in both the plantar fascia and achilles tendon compared to the asymptomatic side. When these findings were compared to asymptomatic controls, achilles tendon stiffness was consistently lower, in the symptomatic group. Importantly, there were also functional deficits in strength reported, including reduced repetitions in the heel rise test and the step-down test. Therefore, stiffness may not be the bad guy after all with the results indicating that pain was associated with reduced stiffness and not the contrary (Rabelo et al. 2023).
I’ll let you reflect on these findings and consider why stiffness may be important is some tissues when considering their functional role. Additionally, and in the context of manual therapy and rehabilitation, is always focusing on reducing stiffness / tone the best approach?
How good are your palpation skills?
We have all had those patients that say, “Can you feel the painful side?” Or “Can you feel how tight it is?” and we respond with something like “Oh yes… of course I can, it’s definitely the left side… right??” or “Maybe it’s the right side…Left?”
If we took away the opportunity for a subjective assessment, and we blindly walked into a clinical encounter, could we use palpation to identify the painful side on a patient? Well, Maigne et al. (2012) investigate this by testing if palpation of muscle tension could identify the painful side in patients with unilateral low back or neck pain. Interestingly, in patients with low back pain, clinicians correctly identified the painful side 65% of the time, which is slightly better than chance. However, in neck pain group, the accuracy dropped to 58%.

What about trigger points?
I know what you are thinking, and you are not the only one. I too have bias about my own skills and experience… But let’s talk about something that we are all very familiar with, the myofascial trigger point (MTrP).
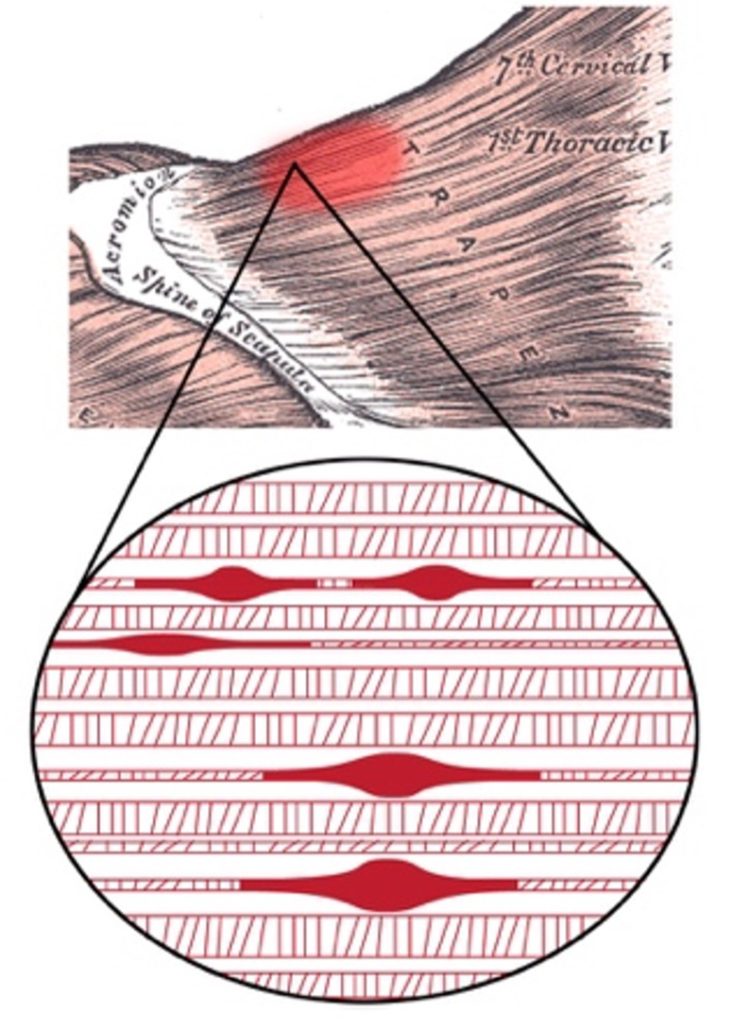
Palpation is a fundamental component of identifying a myofascial trigger points. But how reliable is trigger point palpation? If we just think about this for a second, we are talking about, contractures at the microscopic sarcomere, that’s buried under skin, fat, and other connective tissues … Surely, we don’t get it right every time, do we?
Before reading any further, think about the diagnostic criteria that you use to diagnose a myofascial trigger point?
That’s okay if you couldn’t, because as we turn to the literature, there is considerable heterogeneity in the diagnostic criteria used to identify MTrPs. In a systematic review, examining the diagnostic reliability of MTrPs that included 198 included studies, only 65.1% clearly reported MTrP diagnostic criteria. With many studies not reporting the diagnostic criteria at all. (Li et al., 2020)
Furthermore, in a systematic review and meta-analysis, that aimed to assess the interrater reliability for identifying myofascial trigger points (Rathbone et al., 2017). Localised tenderness and pain were the most reliable measures between different examiners. However, there was only moderate agreement between examiners about the location of the MTrP. This means that if several clinicians individually palpated for a myofascial trigger point, correctly identify the location would be slightly better than chance, however not all would agree that the MTrP is in the same spot. So again, this questions the accuracy and reliability for using palpation in isolation.
What’s my point?
It is important to acknowledge that a tight muscle does not always indicate pathology or dysfunction and may not need to be ‘released’. However, in some cases ‘tightness’ may simply reflect protective muscle activity and certainly can contribute to pain. Additionally, while palpation can be a useful part of an assessment approach to detect areas of pain or sensitivity, over reliance of palpation may risks false confidence and may lead to structural explanation of the tight or stiff muscle being the cause of the pain. This also challenges the explanation that “I am intuitive, and I go by feel”. The narrative of palpating for dysfunctional / tight tissues to direct treatment has limitations when it comes to pain.
Should we still palpate? Yes, it is a foundational skill of all manual therapist, but it should be used as a part of a multimodal assessment process and be mindful to link muscle tightness or stiffness with dysfunction and pain.
References
Barreto Rabelo, D., Coelho Figueira Freire, A. P., Colen Milagres Brandão, F., Oliveira Melo, S., Ocarino, J. M., Saldanha Dos Anjos, M. T., Schleip, R., Souza, T. R., Simoneau, G., & Zambelli Pinto, R. (2023). Myofascial stiffness of plantar fascia and Achilles tendon in individuals with plantar fasciopathy: An observational cross-sectional study. Musculoskeletal Science & Practice, 66, 102781. https://doi.org/10.1016/j.msksp.2023.102781
Li, L., Stoop, R., Clijsen, R., Hohenauer, E., Fernández-de-Las-Peñas, C., Huang, Q., & Barbero, M. (2020). Criteria Used for the Diagnosis of Myofascial Trigger Points in Clinical Trials on Physical Therapy: Updated Systematic Review. The Clinical journal of pain, 36(12), 955–967. https://doi.org/10.1097/AJP.0000000000000875
Maigne, J. Y., Cornelis, P., & Chatellier, G. (2012). Lower back pain and neck pain: is it possible to identify the painful side by palpation only? Annals of Physical and Rehabilitation Medicine, 55(2), 103–111. https://doi.org/10.1016/j.rehab.2012.01.001
Rathbone, A. T. L., Grosman-Rimon, L., & Kumbhare, D. A. (2017). Interrater Agreement of Manual Palpation for Identification of Myofascial Trigger Points: A Systematic Review and Meta-Analysis. The Clinical Journal of Pain, 33(8), 715–729. https://doi.org/10.1097/AJP.0000000000000459

